Genetics, Research, and Future Therapies for NF1 with Dr. David Gutmann
Shane: Hello again, I'm Shane, and this is Decoding NF.
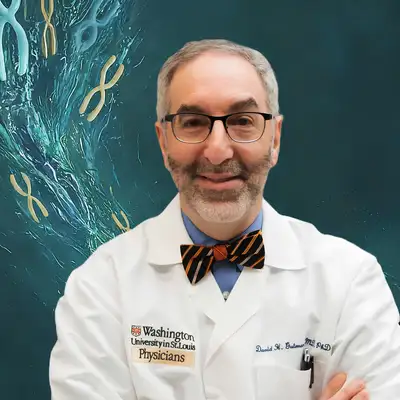
My guest today is none other than Dr. David Gutmann. Dr. Gutmann is a renowned neurologist specializing in neurofibromatosis, particularly NF1. His research focuses on understanding the genetic and cellular mechanisms behind nervous system problems in NF patients. Early in his career, Dr. Gutmann identified the role of the NF1 protein neurofibromin in down regulating the RAS cell signaling pathway, and has since used innovative techniques like induced pluripotent stem cells and engineered mice to explore its function.
He established the Washington University Neurofibromatosis Center, a world leader in the field, and has developed community programs to provide patients care throughout their lives. Beyond research, Dr. Gutmann champions collaboration. He has established international partnerships, led efforts to create medical practice guidelines, and facilitated clinical trials for new NF treatments.
His dedication extends to training, having mentored numerous clinicians and scientists, and actively contributing to educational programs. Dr. Gutmann's achievements are well recognized. He has published over 500 scientific papers, received continuous funding from the National Institutes of Health, and has been honored with prestigious awards, including the 2012 Children's Tumor Foundation Frederick von Recklinghaus Lifetime Achievement Award, a 2013 Washington University Distinguished Faculty Research Award, a 2017 Alexander von Humboldt Award, the
2019 Society for Neuro Oncology Abhijit Guha Award, the 2020 National Neurofibromatosis Network Advocate of Hope Award, the 2020 American Academy of Neurology Neuro Oncology Scientific Award, and the 2020 American Association of Neurology Triennial George W. Jacoby Award. He is an elected fellow of the American Academy of Neurology.
The American Neurological Association, the Association of American Physicians, the American Association for the Advancement of Science, and the National Academy of Medicine, as well as a former member of the National Institute of Neurological Disorders and Stroke Advisory Council.
That is quite a bio. I have been really looking forward to this interview from the moment it got scheduled. Dr. Gutmann is a giant in the field of NF research and I couldn't wait to talk to him. And it was everything I hoped it would be. Our conversation really goes in a lot of different directions. And if anything, I felt like I left with more fascinating concepts and ideas that I wanted to explore than I came in with, and I could have just kept asking questions for hours.
I will say that this episode gets pretty into the weeds a few times and there's a lot of technical stuff around cell signaling pathways that we allude to. I tried to link to a few resources in the show notes that can help ground anybody that is listening to us talk about RAS and RAF and MAP kinase and just feels a little lost.
So definitely check that stuff out. If you don't have a little bit of background with that stuff already, maybe start there before you listen to the episode. But I think that there's enough information here presented in as consumable way as possible to where, even if you don't have that background, you should still get something out of this episode. He also mentions several papers throughout the course of the interview, and wherever possible, I tried to link to those too.
One last technical note, I think that in the software that I used to record these interviews remotely, our audio streams got a little bit out of sync and in the final audio files It has a tendency to sound like Dr.
Gutmann is cutting me off
at the end of the questions as his answers start to come in right as I'm ending the question.
I fixed it where I could, I couldn't fix it everywhere without degrading the quality of the audio. It doesn't actually affect any of the information in the podcast episode. It just causes the interview not to always flow as it should,, and it makes it seem like Dr. Gutmann's cutting me off a bunch, which he didn't during the interview, so I just wanted to make note of it. As always, this podcast is for general informational purposes only and does not constitute the practice of medicine, nursing, or other professional healthcare services, including the giving of medical advice. No doctor patient relationship is formed.
The content of this podcast is not intended to be a substitute for professional medical advice, diagnosis, or treatment, and listeners should not disregard or delay in obtaining medical advice from their doctors.
Okay, one last announcement and then on to the interview, I promise. We have a Patreon! Making and hosting. This podcast isn't free of course, so if you want to help offset those costs and even play a role in the future of Decoding NF, which might mean more frequent episodes or traveling to conferences. Stuff like that. Then go to Patreon.com/DecodingNF or go to patreon.
com and search for decoding NF or go to DecodingNF.Com and of course there's a patreon link there and sign up for the membership
it's only $4 a month. And when you sign up, you'll get access to a members only version of this podcast feed that includes the episodes you can hear for free without this spiel, of course, but a week to sometimes weeks early. And of course, you'll get access to any future benefits of being a member as I add them.
Alright, without any further delay, here's the interview.
Dr. Gutmann thank you for taking the time.
Dr David Gutmann: It is my pleasure. I look forward to talking to you.
Shane: So we're going to go all the way down the neurological road here. As it relates to NF1, but I want to start by just laying some groundwork. So could you talk a little bit about your research background, how you ended up specifically focusing on NF1, and then talk a little bit about how you ended up discovering the function of neurofibromin
Dr David Gutmann: Absolutely. So I was fortunate enough as a resident to fall under the spell of one of our neurogeneticists at Children's Hospital of Philadelphia and the Hospital University of Pennsylvania named Kenneth Fishbeck. And Kenneth really instilled in me a love of the genetics of neurologic diseases. And so when I spent time at the Children's Hospital, where they have two NF clinics.
I really became enamored of these families and really struck by the variety of problems that these kids and young adults face. From there, it was an easy decision of which laboratory to join as a postdoctoral research fellow. And I found my way to Francis Collins Laboratory about the same week that the NF1 gene was identified.
Because the lab was full of experts who focused on the gene and how the gene works. When I came on board, they said why don't you work on the protein and what the protein does? And that was really my beginnings. My charge as a postdoctoral research fellow was to make antibodies, reagents that you could use to identify the protein and with those reagents in hand, we were able.
To both by ourselves and in collaboration with other researchers, identify that neurofibromin as its major function operates to shut off the activity of the RAS gene and protein.
Shane: Okay. That's a great segue into neurofibromin as a protein. It's function. , so when you say it, shuts off the RAS pathway, let's dive into that a little bit more, maybe talk a little bit more about, RAS, RAF, MAPK, that whole cell signaling pathway and how neurofibromin fits into that, and then and then we can talk a little bit more about the specific mutation of NF1 and how that affects neurofibromin.
But let's start with neurofibromin's role and get into a little bit more detail about what
Dr David Gutmann: So once we had the reagents to study neurofibromin, the protein, what we first focused our energies on was a very small region, perhaps 10 percent of the entire NF1 protein. that looked like a family of proteins whose primary function it was is to shut off the activity of the Ras protein. And what Ras does is as a driver of cell growth, it talks to a diverse number of proteins downstream of Ras to communicate that message that the cell should grow faster.
There are a number of these pathways. The one that has gotten the greatest attention over the past 10 years has been the RAF MAP kinase pathway. And the reason it's gotten so much attention is that there are inhibitors. RAF, there are inhibitors of the MAP kinase signaling pathway. that were in clinical trials for other disorders that got repurposed and used to treat individuals first with plexiform neurofibromas and more recently optic gliomas and further down the road learning disabilities in kids with NF1.
Having said that, we're still talking about 10 percent of the entire protein. And Mother Nature is pretty conservative of how she uses genes. And to make a protein that is ten times larger than it needs to be seems as if we might have missed some of the other functions of the NF1 protein. So there are other functions that have gotten less attention that are particularly relevant to how NF1 works in the brain.
They include cyclic AMP. They include regulation of dopamine, they include regulation of excitability of neurons. And so while we have some early clues as to how neurofibromin might function as a RAS regulator, there's still other functions of neurofibromin that have not been unraveled.
Shane: So there you're alluding to maybe some of the neurological effects of NF1 like with learning disabilities and behavioral disorders, things like that. When you talk about maybe some of the other roles that neurofibromin plays that are
just not super clear yet.
This really interests me and I'd like to take a little bit of a detour down that road if we could.
We've got a ton of stuff to cover, but from a research standpoint what kind of clues are we getting as to what role neurofibromin might play when it comes to those behavioral disorders and to neurons on a kind of a structural level, is it related to the same way that, that you get nerve sheath tumors , in NF1 patients does the quality of nerve sheathing and things like that.
Does that affect cell signaling in between neurons or what is the thought there if there is any yet as to how that mechanistically
Dr David Gutmann: So we have spent the better part of a few decades focused on how neurofibromin absence or dysfunction leads to increased RAS signaling in tumor cells. And so most of what we know is focused on tumors where neurofibromin is no longer expressed. What we have less of an appreciation for are the impacts of.
NF1 mutation on nerve cell function, immune cell function, and oligodendrocytes, Schwann cell like cells that ensheath nerve cells in the brain. When we and our colleagues have looked the ways that neurofibromin functions in these different cells, it's not always RAS MAP kinase in neurons. The length and the sprouting of a neuron, how it forms connections is mediated by cyclic AMP.
Its ability to communicate with other nerve cells by controlling the release of neurotransmitters is RAS independent. And finally, the activity that is the firing rates of nerve cells with an NF1 mutation is increased. Which is also independent of neurofibromin's ability to regulate RAS. So just in the neurons alone, we now appreciate that it's not all about RAS and it's not all about RASMAP kinase.
And then finally, in a collaborative study with Michelle Monje's lab, published just a month or so ago, we showed that in sheathing cells, the oligodendrocytes are impaired when there's an NF1 mutation. And that does not operate through MAP kinase. It operates through AKT, another molecule downstream of RAS, but in this case appears to operate independent of RAS activity.
So as we've gotten smarter about how NF1 loss in tumor cells can be targeted by shutting off the RAF MAP kinase pathway, we now appreciate that. Other functions, and particularly functions relevant to learning, behavior, autism, may be mediated by other properties of neurofibromin besides and beyond its ability to regulate RAS.
Shane: That's a kind of a common effect in oncology, isn't it? Where we find we'll use a type of chemotherapy to target a specific cell signaling pathway to downregulate something. And then we find that the cancer cells metabolism works around that some of the time. I'm wondering, do we find that to be the case in NF1 tumors that as you down regulate like MEK1 and 2, for instance, which is the current way that we're down regulating the MAPK pathway in NF1 anyway that it will, work around that at all? Or do we find that it remains effective regardless?
Dr David Gutmann: There are two different questions that I'm going to answer. disentangle. One is the adaptive properties of tumor cells. So you're correct that tumor cells, when they're exposed to high levels of inhibitors of say the RAS or MAP kinase pathway, can develop escape routes where they overcome the suppression that's mediated by the inhibitors.
that does occur. It tends to occur a little bit more in malignant tumors. There is some rebound and resistance that can occur in the setting of RAFMAP kinase signaling. The other question that I'm going to allude to that you didn't mention is what are the cells in the tumor microenvironment contributing to tumor growth.
And that we've spent decades studying. In my laboratory and in other laboratories. And what's very clear is that those non cancerous cells are absolutely required for tumors to form and for them to be maintained. So the next generation of treatments are going to focus not only on the MAP kinase pathway, which is what's used by the tumor cells to grow.
But to find ways to disable the tumor microenvironment, whether it's immune cells or nerve cells that contribute to tumor formation and growth
Shane: so is it, wasn't that kind of the idea behind the use of Ketotifen , and the idea behind mast cell death regulation in the eighties that didn't really prove out in NF research. I get, are we coming back to that same
set of ideas?
Dr David Gutmann: Let me talk about that and then I'll, we'll move to brain tumors for a second because I think what you bring up is a brilliant observation by the late Vic Riccardi. Vic Riccardi was an exemplary physician who noticed that folks with NF1 associated neurofibromas, the cutaneous Tumors that arise on the skin often complained of itching as their tumors were growing.
And he asked whether or not it is possible that immune cells, in this case called mast cells that release histamine and cause itching could contribute to tumor formation and growth. And that's where Ketotifen came in. And because it wasn't a well controlled study, it was ignored for 20 years until Wade Clapp's lab showed that mast cells in mice drive tumor growth.
And then Imatinib and other related drugs became available in the 2000s to target the mast cells and non cancerous cells in the tumors for plexiform neurofibromas. What we're appreciating now is that's also true for brain tumors. And work from my group has shown that immune system cells and neurons communicate with each other.
to support the environment that is conducive to tumor formation and growth. And if you target immune system cells or nerve cells, you can abrogate tumor formation and growth because they're so dependent on their microenvironment, which now means you have additional alternative strategies or adjuvant therapies that we can use in addition to MEK inhibitors.
That, might really expose an Achilles heel for those tumors and stop them from growing in a much more durable fashion.
Shane: And when we talk about the tumor microenvironment here, and I know in your case, we're specifically talking about brain tumors, mostly right. And maybe optic pathway gliomas. What is that microenvironment made up of? How exactly does a tumor function in that
Dr David Gutmann: So tumors, like all of the cells in the body, have to function within a tissue and cells always communicate with each other in order to maintain a certain level of homeostasis within a tissue. And to respond to injury and repair itself. And that's true for the developing skin. It's true for the developing brain.
There's always an interaction between these cells. What you've done in the setting of a tumor is you now have one population of cells that are growing faster and inappropriately. But there's still a lot of other cell types that are not cancerous that normally would interact with, whether they're neurons or mast cells or Schwann cells.
They're necessary for the communication and they are just simply being subverted to promote the survival of the tumor. So tumors have just usurped The normal communication between cells to tip the advantage for their own survival and growth.
Shane: Let's get into the specifics about, the manifestations because I feel like we went far afield a little bit. Let's go back to basics. In the case of NF1, what are the neurological manifestations, the neurological pathologies associated with NF1? Let's just start there and then maybe we can talk a little bit about each of them specifically, talk about their standard of
Dr David Gutmann: Absolutely. If you see folks in clinics, particularly children, the most common neurologic problem are really going to be learning problems, attention deficit and autism spectrum like features. The next most common thing we'll see are Brain tumors and specifically brain tumors that arise along the optic pathway that connects the eye to the brain.
And then we'll see other tumors that arise in other regions like the brainstem. Kids can also have seizures at a slightly elevated risk, sleep problems and they are also prone, although at a smaller fraction to blood vessel abnormalities in the brain that can lead early stroke and devastating neurological consequences.
Shane: Let's talk a little bit about Some of those. So in the case of the behavioral disorders and attention deficit, things like that, is the standard of care for NF1 or rather maybe even because the standard of care is the same as anyone else with ADHD, I guess, but based upon your research, is there anything coming along that might differentiate NF1 kids from say more idiopathic version of ADHD and a quote unquote, normal kid without, without an NF1 mutation. Is there anything that will change by the way that we treat NF1 behavioral disorders versus just, some other kid that is otherwise genetically
Dr David Gutmann: So you're, you're right. Today we treat kids with NF1 and autism, attention deficit learning disabilities, the same that NF1. If you can extrapolate from genetically engineered mouse studies, what's pretty clear is that there are differences in the levels of particular neurotransmitters. Alcino Silva's group at UCLA has focused on a particular neurotransmitter called GABA, and there are drugs out there that can change the ability of GABA to function.
We have focused on dopamine, and in particular because of its relationship to attention deficit or anxiety. And in that case, The mice with an NF1 mutation have lower levels of dopamine in their brains, and when we restore that using drugs that we would treat folks who have low dopamine levels, like folks with Parkinson's disease, we can reduce the amount of attention deficit that we see in a mouse.
We don't have any idea today, what's different about autism or cognitive problems in folks with NF, despite many years of study, it's not clear what makes them different from folks who don't have NF1. We've looked very carefully at autism and everything about how autism behaves in the general population appears to hold true for kids with NF1.
with the one or two exceptions. One is that we see boys and girls more equally affected in the setting of NF1, whereas in the general population, boys are much more frequently affected. And second, we tend to make the diagnosis of autism Later in folks with NF1 than we do in the general population.
There's work ongoing in many groups trying to discern whether or not that's a difference in how the brain is wired in kids with NF1 versus the general population. And how can we use that information. to design medications that might be more effective for those kids specifically with NF1.
Shane: I want to ask a little bit about longer term neurological impacts of NF1. You mentioned, only because you mentioned something about dopamine deficiency in NF1 patients, and I'm wondering, over the long term, something like that being untreated, does that lead to, say faster age related cognitive decline or or dementia? Any of those types of effects noted in NF1 adults as they get older? Are they at higher risk for neurological disorders
Dr David Gutmann: do appear to be and those are not cause and effect studies, so I can't prove that having NF1 in lower dopamine levels or difference in the way the neurotransmitters behave is What causes more dementia, depression Alzheimer's disease, Parkinson's, than I would see in the general population.
All I can say is there, there's a slightly increased number of folks with those neurologic disorders when they're adults than we would predict in the general population.
Shane: That's interesting. And then I want to ask about the exogenous dosing of GABA. Does that have any effect on NF1 patients? Or do we need to just focus on drugs, prescription drugs, that can increase the endogenous production
Dr David Gutmann: So for dopamine, the levels are lower. For GABA, the levels are higher. Uh, And
Shane: Oh, Oh,
I didn't understand.
Dr David Gutmann: uh, Much more work is going to be required before we start treating folks with GABA inhibitors. There's been one small study using dopamine elevators, drugs , that allow for more availability of dopamine in the brain.
In kids who have learning disabilities and attention, and at least in that one study, there was a benefit of taking these, this medication for the attention deficit, but not so much for the cognitive problems.
Shane: Because of the differences in How NF1 kids, come to having ADHD as a pathology. Do we find that the stimulant based approach that's taken with most ADHD is less effective with NF1 kids? Or is the standard of care for ADHD still basically effective for NF1 kids? kids. Do we need to adjust, if I'm a parent with a, with an NF1 kid that, that has a behavioral disorder, has ADHD, for instance should I be, adjusting my approach or thinking about that any differently
Dr David Gutmann: at
this point, there's no evidence that we should treat kids with NF1 and attention deficit any differently than we treat folks in the general population. And so our, approaches are behavioral and then at least as first line using medications that readjust the brain chemistry just like we would in, in kids who do not have NF1.
Shane: Okay. Let's talk about current standard of care for NF1. And then I want to talk about what in the. shorter term and longer term future as it relates to the neurological effects of NF1. So MEK inhibitors are still the standard of care for NF1, I think, at this point. Is there anything else that is either immediately on the horizon or currently in use for kids with NF1? either optic pathway gliomas or brain tumors or other neurological focused pathologies.
Dr David Gutmann: So I think we need to take a little bit of a trip down our, down history here in order to put the MEK inhibitors into context. Because the first medications that were rolled out when it, We recognized that NF1 was a RAS regulator, were medications that targeted the RAS molecule and RAS's ability to signal.
And then we realized that RAS talks to another protein called the mechanistic target of rapamycin or mTOR. And so we went through a series of mTOR inhibitors, and then we recognized that maybe the more efficient pathway was RAS to RAF to MAP kinase. And that's where we are now, where we use it for treatment of plexiform neurofibromas in kids and adults.
And we're beginning to use it for optic gliomas and low grade brain tumors in uh children with NF1. That reflects our evolving understanding of how NF1 loss in the tumor cells might be responsible for increased cell growth. As we've learned a lot more about what is important for maintaining the tumors, and I'll speak for a second about optic gliomas, we now appreciate that the immune system plays a critical role.
So a medication that's now in clinical trials is to interrupt that immune system stimulation that would support the tumor. So that clinical trial is in its very beginnings. We have a second clinical trial that's still in the conception form and has been presented, vetted, and is being discussed as a clinical trial.
And that's based on the fact that nerve cells, in particular the nerves in the optic nerve, when they have an NF1 mutation become more excitable. And by repurposing a drug that we use to treat epilepsy, we've been able to shut off that excitability and get the tumors to stop growing. That's now being discussed as a next line therapy, perhaps to prevent tumors from growing.
growing and developing and to obviate the need for definitive chemotherapy in kids who have NF1 optic gliomas. And you can imagine as we learn more about the circuits that maintain these tumors, not just the tumor cells, we'll have much more creative next generation therapies that are based on a true understanding of how these tumors form and how they're maintained and how they escape our therapies.
And that's where I think the future really is so exciting.
Shane: That's interesting. So maybe we can talk a little bit more about the future in somewhat concrete terms. Based upon the research that you see or that's About to go into trials or, based on what you know what do you think the next, say five years holds when it comes to NF1 treatment? And then maybe we can even go a little bit farther out if you're comfortable doing that as to, where the most effective treatments are probably going
Dr David Gutmann: Right, So I think the two biggest challenges we face in managing children and adults are the unpredictability of the condition, and the lack of control. Truly specific therapies when problems need to be addressed. One major change in our ability to better care for folks is going to be to identify predictive biomarkers for specific problems in NF1.
That's something that we have tackled and continue to work on with bioinformaticians in our Washington University Institute for Informatics, to use AI and machine learning approaches to extract information from the medical records, the imaging studies, genetic studies, to try to predict for any given patient whether they're likely or not likely to develop an optic glioma or attention deficit.
That would be game changing for our families because they wouldn't be necessarily waiting for the second shoe to drop. They would have a much better idea of how to tailor our anticipatory management, our screening for particular medical problems by focusing our resources on those kids that are at the highest likelihood of any particular medical problem.
The other thing that would be an amazing change in the way we manage folks with NF is to stop thinking. about every medical condition as being caused by dysfunction of a single cell. I think we need to move away from the idea that learning disabilities are about how NF1 works in one neuron or two neurons.
We need to move away from the idea that tumors are all about MAP kinase signaling in the tumor cells. And that these are all circuits where cells talk to each other, support each other, and propagate the disease when in the setting of NF1. And as we begin to have a different conceptual approach, it's obvious to me and probably to others that some of the therapies may be much more refined and much more likely To have long term, durable effects, because we're really attacking the tumors or the learning disabilities at the root of the circuits that maintain them.
Shane: I completely agree and I think that is one of the really genius insights that doctors like Riccardi had is thinking of NF as a complex system rather than being a, a series of manifestations that you've got to, play whack a mole to knock down. But I wonder how much of that is just the tools available.
So we're at a point now with, Machine learning, large language models, things like that, where we can actually conceptualize and potentially even start to make some of those predictions that you're talking about of the impact of a specific kind of NF mutation and how that will have an effect on the complex system of the body. And do you feel like that is something we're slowly getting to that point where we can start to. make those kinds of predictions reliably? Or do you think that's still, maybe a decade off or something like that, what is your thought on how much that will become a tool in the toolkit for the average NF patient in the near
future?
Dr David Gutmann: think it's decades off, I think it's years off. So we've already built some predictive models that are performing. absolutely well at Wash U. We're bringing them to other institutions to see whether or not they function well in other institutions so that we can refine them so that they'll be useful regardless of where the patients are.
I think it will have to incorporate a lot of different information. So work in my lab is particularly focused on risk factors, but you can't conceptualize risk factors. unless you know how they operate and how they converge on the circuits that maintain tumors or learning disabilities or attention deficits.
And once you have circuits that you can delineate, you now can figure out how those risk factors work. And once you figure out how they work, you can provide some weight to their So are they highly predictive? Weakly predictive? And do they also become tools for us to attack the condition in terms of therapy?
And I see a very exciting next five years because we're already beginning to move beyond that. a simple genotype phenotype correlation. It's not going to be that simple. It's going to be the coalescence of multiple factors that allow you to see very specific patterns of risk in people with NF1.
Shane: And you think, so you think that'll become more widespread. I think at this point, from a genomic standpoint, I don't think the average NF1 patient. I think a lot of diagnoses are made strictly by, external pathologies or maybe familial background, that sort of thing. Do you think that the genomic component then of just for the average patient will become really critical in the next like half decade then. And you think some of those applications will come out of research centers like yours and make their way into the general standard of care then? Is that what you're
Dr David Gutmann: So, The first thing we need to be able to prove is that the genetic mutation is predictive or that the genomic alteration or variation confers a different level of risk. And those are going to be either laboratory studies or translational studies that are really going to require thousands and thousands of patients to make sure that they are highly reproducible.
Once that succeeds, then I think we can start to talk about integrating them in daily practice. But again, you need to go back through our history of NF1 logic. For the longest time, people said a mutation is a mutation is a mutation. It doesn't matter. They all lead to dysfunction of the NF1 gene. And the reason they all lead to dysfunction of the NF1 gene is every single one of them appears to lead to dysregulated RAS activity.
It's now been over a decade where we were one of the first to show that actually different mutations While conferring the same level of RAS dysfunction, had profoundly different effects on brain development, on neurotransmitters, on optic glioma and plexiform neurofibroma formation in mice. And now, people are wrapping their brains around the idea that mutation might actually matter.
Fast forward a few more years, as we accumulate more of that genetic data. Fast forward. Based on our evolving notion of, what a mutation means, we will have more genetic information to test these hypotheses and then evaluate whether they have real time utility in a clinical setting.
Shane: Yeah I see what you're saying. It's just this idea of slowly evolving the thinking around NF from, the idea that, a mutation has these second and third order effects. When we've already known that you know, the whole thing, if you've met one NF1 patient, you've
met one NF1 patient, right? And why large animal models were so difficult for so long, , because you can replicate a pathology or two pathologies or whatever, but, replicating quote unquote NF1 in an animal model has proven to be pretty difficult. And so again, if you're working off of an animal model that has say, two or three pathologies related to an NF mutation, right? And you're, so you're developing treatments or protocols for those manifestations by its very nature. You're not really working from the source down. , So, are you saying that we're going to get to the point where, as we've moved closer and closer to working up from the external manifestations of NF1, all the way up to what's causing them at a systematic level,
That we're eventually going to get to the point where we can treat them at that same systematic level.
Dr David Gutmann: Yeah.
So I guess there need to be a few changes and it's normal evolution of a field. We need to take our available data and ask whether it still fits the simplistic models that we concocted when the gene was first identified or The first clinical trial started and as we evolve from RAS to MAP kinase to maybe other drugs, from a single cell to multiple cells in a circuit, we begin to think about the problem differently.
And it's not simple. But it can be simplified, and I think we have to generate models that are more reflective of the diversity of the patients that we see. And until we recognize what contributes to diversity, that is, it's not just a tumor cell that has NF1 loss. And if we study it in one mouse, we don't need a second mouse, because all we're modeling is.
NF1 loss in the tumor cell. As you begin to appreciate that's not enough to account for the diversity and you layer on immune system cells, neurons and whatever, you now have to think about the problem differently. And by thinking about the problem differently, you will have new approaches.
You will have new platforms for testing drugs. That maybe have to incorporate numerous models in order to truly capture the kind of variation we see in our patients. And we need to be able to layer on that what other differences are there in our mice, our pigs, our rats, that contribute to the variation that we see in people.
And some of those, I believe, will be actionable, not only in terms of risk assessment. But in terms of therapy,
Shane: That makes sense. You're thinking like, the combination therapies that are being experimented with, like the SOS1 inhibitors, along with MEK inhibitors, will learn with more granularity when to apply those particular things, rather than having a blanket approach, say for NF1 patients with plexiform neurofibromas, we'll be able to be a little bit more personalized, a little bit more specific. And so that leads me to the thought, I wonder, do you think then that there will be some kind of differentiation with NF1 in the way that, NF has already undergone this recent terminology change from, you know, , schwannomatosis to, NF2 related schwannomatosis, et cetera, as the understanding changes.
Do you think NF1 will eventually differentiate into multiple disorders at that point that each have a different kind of genomic profile? Do you think that's appropriate?
Dr David Gutmann: I don't know that we need to subdivide NF1 into new disorders. Where I think our second generation, third generation thinking might really benefit is when we move away from the idea that will fix the problem by just targeting the same pathway better or at multiple spots. That at some point you have to say maybe that's not the complete answer and maybe not everybody's tumor is completely dependent on MAP kinase or RAF.
Maybe there are other dependencies that subdivide tumors into different therapeutically actionable subgroups. But we need to be able, this is where, you know, AI becomes really helpful, is that when you're in the clinic, a plexiform is a single plexiform in a patient. You can't put it in the context of the other hundred plexiform neurofibromas that you see in your patient population.
But AI can see all, AI has the ability to see thousands if not tens of thousands of variables at the same time, and regroup patient tumors by their features that we would never be able to do, seeing one patient. So I think we have, I think it's gonna be a conceptual change. It's for the, the field in terms of how we're thinking about.
what the etiologies are for tumors and learning disabilities and other clinical manifestations. It's going to be about how we envision risk factors to work. And then it's going to be about how we're using the models that we need to translate basic science discoveries into the clinic more effectively so that they actually represent.
the diversity of the patient population. So we don't throw out good drugs that work for a small proportion of folks with a particular problem. And we don't embrace drugs that only work for a small proportion, but don't really serve the greater good.
Shane: Yeah, right. they might inform the kind of the RCT process in terms of rather than just recruiting NF1 patients, you might recruit NF1 patients with a particular kind of genomic profile. Is that what you're thinking?
Dr David Gutmann: Well, You just don't know what
you're looking for. You know,
It's very difficult for the human brain to see all the factors in any given patient. There's just no way for me to wrap my brain around it. The diet, the other medical problems, the mutation, the genomic alterations, the location of the tumor, there's hundreds, thousands of variables.
I'm not going to be able to classify my patients in an unbiased way, seeing one patient at a time. And that's where, having these advanced computational tools will, could transform the field and allow us to think about things differently.
Shane: I want to talk a little bit about the field, a topic that's come up a few times, just in various conversations is around. The future of NF research in general. And I'm wondering, how do you feel about luminaries like Dr. Riccardi passing away.
And I think Dr. Korf is, moving on from the role that he held for a long time. Do you feel like we have a good kind of bench of clinicians and researchers coming into the field to expand that understanding to pass those torches on and keep that research going. I've heard some concerns here and there that, just in general, medical residencies are having trouble filling in particular fields. And I'm wondering if that's affecting NF1 research at all, or do you think it might in the
Dr David Gutmann: So as somebody who's worked on NF for nearly 35 years now, I get up and I'm still excited about the future. The, it has been nothing but an amazing trip to watch us evolve over the years in terms of how we take care of families. We had no practice guidelines when I got started. We have practice guidelines.
We have. Medications. We have imaging studies that we couldn't dream of doing, of using before. It's a totally new world. Those of us who have had the pleasure of training the next generation of practitioners and researchers, are just amazed by what they will do when we ride off into the sunset.
I don't see, I don't see us ending NF investigation anytime soon. I think if anything, the future is incredibly bright as we have probably the most dedicated group of researchers who are really focused on. understanding the complex biology of NF today than we've ever had.
Shane: That's great to hear. I think as we're coming up on time, that's a great kind of optimistic note to start to wrap things up. But before we go, I want to be respectful of your time. I know you're, you're super busy and I appreciate the time that you've already given me. So before we wrap up, I just want to ask you if there's anything else that we didn't get to that you really wanted to talk about or anything else you'd like to part with before we end
this
Dr David Gutmann: you've covered almost all of the topics. I think the one thing I wanted to make sure I emphasized was what we just talked about. We have, not only have we learned so much about NF, but we've taught the world so much about other conditions. Based on studying NF and it is really one of the true pluses of working in a field like NF is that the principles that underlie NF are applicable to so many common medical conditions and can really inform how we take care of folks with brain tumors, how we can take care of folks with autism.
in ways that those fields have never thought of before. And so I think of NF as a lightning rod for change, that we have the ability not only to completely revamp how we think and care for folks with NF, but also in a small way, revolutionize how we take care of folks with other common diseases.
Shane: Yeah, I will say that I've had a similar kind of evolution in that, as my understanding of NF grows in general, I make a lot of connections to a lot of other, understandings and a lot of other things that I just didn't know before that I find super interesting.
And NF is such a, because it's such a I guess, systematic disorder that affects so much of how the body functions. There's just to wrap your head around it, even at a conceptual level, there's just so much that you need to understand about it that naturally leads you down all of those little tributaries and rivulets until you end up with a much more complete understanding than you started with at a general level. And so I appreciate that about NF as well. I think it makes clinicians better, and I think it makes
researchers better researchers.
Dr David Gutmann: Absolutely.
Well, This has been great. Thank you so much for taking the time to chat with me.
Shane: No, thank you. I really appreciate it. And I will make sure that we have a link to the NF center in your show page. And if there's anything else you'd like to, for me to make note of in the show notes, please let me know. And again, thank you so much for your time. Thanks again, Dr. Gutmannn.
And, hopefully, maybe in a few years when some of the exciting stuff you're talking about bears fruit, we can come back and have another conversation about new therapies that are emerging from all of this,
uh,
incredible research.
Dr David Gutmann: It would be my pleasure. You take care of yourself. Thank you so much.
Shane: And that's the episode. I want to thank Dr. David Gutmann, of course, for lending his time and expertise. And I also want to shout out Drusilla Jenkins, the project manager in the Department of Neurology at WashU. They were super helpful in getting all this coordinated and rolling with some scheduling changes.
And you know, project managers don't get enough appreciation. So, thank you very much for all of the help.
And of course, I want to thank all of you for listening. You can find. Everything about this episode at DecodingNF. com, as well as our entire back catalog and all of the links to all the places where you can subscribe and listen to this podcast. If you have some thoughts about this episode or any other episode, you can email me at shane@decodingnf.com or we're also on multiple of the media's social like Facebook and Instagram and the social media network formerly known as Twitter. So feel free to reach out there as well. We've got some really awesome episodes coming up through the rest of the year, So make sure that you're following us somewhere, so you get alerted when those drop because they're going to be great.
And of course you can become a member at Patreon.com/DecodingNF to get those episodes early and support what I do. Until next time, goodbye!
Creators and Guests