The Art and Science of Facial Reanimation--A Deep Dive with Dr. Tessa Hadlock
Shane: Hello and welcome
back to Decoding NF.
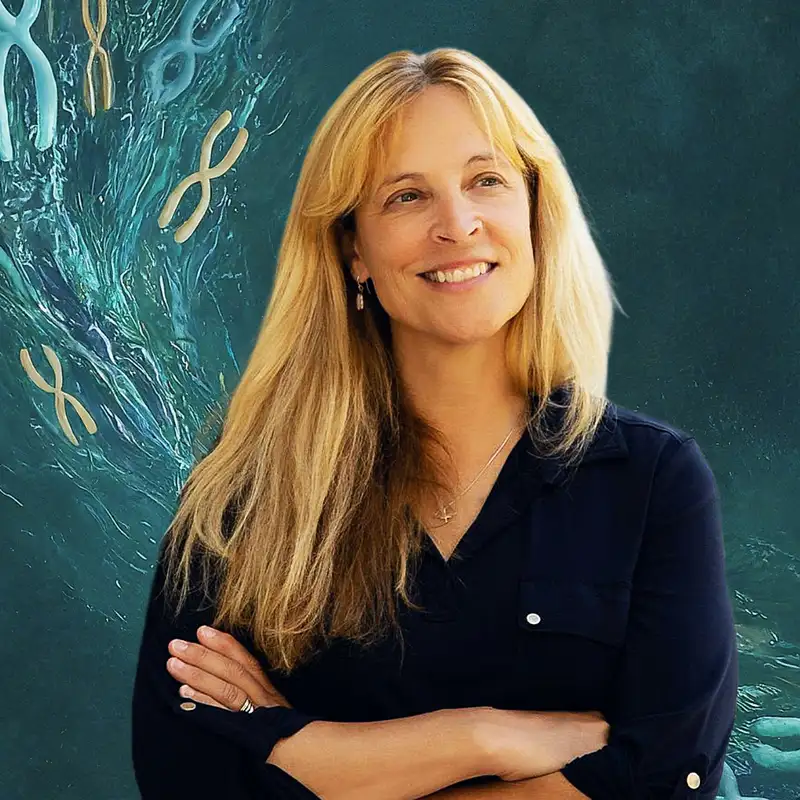
My guest today is Dr.
Tessa Hadlock.
Dr.
Hadlock is a distinguished facial plastic
surgeon and a leading expert in facial
nerve disorders known for her pioneering
work in treating facial paralysis.
With nearly three decades of specialized
experience, she has developed cutting
edge surgical techniques that have
set new standards in the field.
Dr.
Hadlock is a professor at Harvard Medical
School and previously served as the
director of the Facial Nerve Center at
Massachusetts Eye and Ear before founding
her private practice, the Hadlock Center
for Facial Plastic Surgery in Boston.
Her contributions to medical research
are internationally recognized and she
remains deeply committed to mentoring
the next generation of surgeons.
Fluent in several languages, Dr.
Hadlock combines clinical
excellence with a compassionate
approach to patient care.
This was a surprising and super
fascinating discussion about a
topic that I was completely unaware
of until I learned about it from
my conversation with John Manth.
When he mentioned the idea of
facial reanimation, it was a
concept that blew my mind and I
immediately knew I wanted to get Dr.
Hadlock on the show to fully explore it.
And fully explore it we do.
I think this episode serves as a
great primer on facial reanimation
treatments and strategies, both
in how it relates to NF patients,
Mostly NF2 related schwannomatosis,
but also in general.
We cover the major invasive and
noninvasive intervention options for
facial paralysis, both from a functional,
but also a cosmetic standpoint.
And importantly, we talk about
risks and outcomes quite a bit,
which I think is really important.
In NF treatment, we're often
choosing between difficult options
with uncertain outcomes, but this
is an area where the relative risk
to benefit ratio can be really high
in terms of quality of life, and Dr.
Hadlock has spent her entire career
trying to track and quantify the
results of the intervention she
engages in, so I thought it was a good
opportunity to explore that aspect
in a way that we don't always get to.
As always, the content of this podcast
is for general informational purposes
only, and does not constitute the
practice of medicine, nursing, or
other professional healthcare services,
including the giving of medical advice.
No doctor patient relationship is formed.
The content of this podcast is not
intended to be a substitute for
professional medical advice, diagnosis,
or treatment, and listeners should
not disregard or delay in obtaining
medical advice from their doctors.
One last thing, Decoding NF has a Patreon!
For just $4 a month, you can support the
show and you get episodes like this one.
As soon as they are done being edited,
which is usually a week to two weeks
before they go live on this podcast
feed so please consider joining.
You can find more details
at Patreon.com/DecodingNF,
or just go to decoding NF.
com and There's a link there right in
the top navigation for the Patreon.
And of course, in the show notes,
if you're listening to this on
a podcast app, there's a link
to the Patreon in there as well.
Without further ado, I hope you
enjoy my conversation with Dr.
Tessa Hadlock.
Dr.
Hadlock, thank you for joining me.
So I just want to start with a little bit
of your background and how you ended up
in facial paralysis surgery specifically.
Dr Tessa Hadlock: So I was always really
interested in surgery because I grew up
in a very kind of a manual household.
And when I started to focus on
surgery, I recognized that the area I
loved the most was the head and neck.
And then once I got into head and neck
surgery or otolaryngology, the thing that
drew me in so much was facial surgery.
And I think the problem of facial
paralysis was absolutely alluring
because not only does it involve
facial aesthetics, but also
facial function, human function,
and nonverbal communication.
So it had this trifecta of
issues that really attracted me.
I feel like that is the real
reason why I wound up spending my
entire career on facial paralysis.
Shane: I want to drill down into
facial paralysis and NF2 specifically.
But before we do, I think I wanted to
just, I was I don't think I've ever,
and I've talked to a lot of NF2 patients
as well, and I don't think most people
really are aware that something like
facial reanimation is even possible.
And I wonder what your thoughts are
in terms of, why this kind of surgery
isn't, I don't know, more well known.
It seems like a lot of NF2 patients, they
may have a nerve issue or something, and
they don't even realize this is an option.
Dr Tessa Hadlock: Yeah, I
absolutely appreciate that comment.
I think that there are so many diseases
that result in facial paralysis
and NF2 is one of those dominant
diseases that can result in facial
paralysis on one or both sides.
And the problem is that people, both
patients and doctors get so focused on
the disease itself and the natural history
and managing advancing disease, that they
forget sometimes that quality of life
is the fundamental pillar upon which a
lot of our therapies should be based.
And so they, overlook that there are a
lot of short climbs for a long slide where
we can give people a really significant
benefit with surgery that, or not even
surgery, sometimes minor interventions
that can really improve the way that
they express themselves on the face.
It's just overlooked.
It falls in the shadow of
the more dominant medical
issues in the disease process.
Shane: Yeah, I was talking about this.
We did an episode about pain and NF
and it's, this really echoes that,
which is that there has been so much
focus on just trying to resolve the
pathological kind of nature of NF.
NF1, NF2, et cetera.
Because we've been losing for so long,
in that respect, there's been so few
therapies that actually treat it that
the actual quality of life question
really does take a back seat, both in
mental health and in, in stuff like this.
I think this is a really interesting
and to me, unexpected pathway
to that quality of life question.
so when John Manth referred me
over to you to talk about this.
I was cause he mentioned, oh yeah, we did
this facial reanimation surgery, I was
really like blown away by the concept.
It just had not occurred to me.
And partially that is
because of my experience.
I've never had to deal with anything
that involves facial paralysis.
And so I just wouldn't be exposed to
it, but also I'm in the NF community.
I just had not come
across it conceptually.
So I was really interested
to, to explore this further.
Let's talk a little bit about NF2 and
when you have an NF2 patient that comes
to you with some kind of facial paralysis,
nerve damage in the face, what's
usually driving that for NF2 patients?
Dr Tessa Hadlock: Yeah.
Absolutely.
One, one other point I really want
to make before I answer this question
is that when you ask why it's not at
the forefront why facial paralysis
management isn't at the forefront,
another thought that came to me as you
were just speaking is that oftentimes
patients are led toward different avenues
to pursue therapy if their physicians
or their physician team brings them to
the realization that there are things
that can be done about these things.
And I actually think that in NF2 patients,
their primary points of contact are their
neuro oncologist or their neurosurgeon.
And the problem is that sometimes
that group isn't as aware of all the
different things that can be done.
or their experience has been that
a lot of those surgical therapies
haven't been that successful, so
they don't want to push those.
So that was just to add to your prior
thought about why there's a hole in there
that we're, that I would love to fill,
and I think we as a facial reanimation
community want to fill over time.
But getting to the question that you
just asked in terms of NF2 and how and
why it results in facial paralysis,
there are so many different reasons why.
An NF2 patient might
develop facial paralysis.
The most common thing is having
surgical therapy or radiation therapy
for an existing vestibular schwannoma.
That's like the number one
condition that results in usually
transient facial paralysis.
But there are a number of other
situations in which an NF2
patient gets facial paralysis.
For example an actual primary facial nerve
tumor related to the disease process.
So I've had patients where there was a
middle ear mass and a surgeon went after
that mass and ultimately it proved to be
an NF2 related tumor that then sacrificed
the facial nerve because it wasn't
recognized that was the actual tumor.
The facial nerve mass.
Shane: Now, is it always Neurological in
nature or is there sometimes a vascular
source to kind of facial paralysis or
other things in the face like that?
Dr Tessa Hadlock: It's almost
always a neural source.
So the facial nerve either gets damaged
because it's collateral damage to neural
surgery that's adjacent to the facial
nerve or it's damage to the facial
nerve or iatrogenic or intentional
sacrifice of the facial nerve for an
enlarging tumor within the facial nerve.
However, in NF1 and other conditions,
sometimes there are massive
facial tumors in that directly
involve the facial musculature.
And when that happens, it's not really a
neural problem, but rather the end target
muscle that either needs to be resected
or gets directly invaded by tumor.
Shane: That's interesting.
I was thinking of this as an NF2 kind
of problem primarily but I didn't
really even consider the fact that yeah,
it can affect NF1 patients as well.
Maybe a smaller subset
I would imagine though.
Dr Tessa Hadlock: Absolutely,
A smaller subset, but it's
definitely real in NF1 patients.
And it's, I think, talking about
facial reanimation is relevant to
that community as well, though not
as relevant as in NF2 patients.
Shane: So I want to dive into
treatment options then for a patient
with facial paralysis due to NF2.
Is there anything that
characterizes facial paralysis
with NF patients in particular?
Is there anything unique about
the pathology that they experience
or is it all mostly of a kind?
Dr Tessa Hadlock: There are a
couple of unique aspects of facial
paralysis in the NF2 population.
The first two that really come to mind are
number one, patients tend to be younger
when they experience facial paralysis.
And that is a good thing
for facial reanimation.
So a young patient.
or a middle aged patient with
NF2, I tend to think of them as a
very healthy crowd compared with
patients with other conditions
that result in facial paralysis.
For example, head and neck cancer
patients who often don't have the
same Fundamentally healthy substrate.
So they tend to be patients in whom facial
reanimation is actually slightly more
successful than in other populations.
They don't tend to have the vascular
disease that we see with smoking and other
lifestyle changes that can give unhealthy
donor vessels to free flaps, which is
one surgical option for facial paralysis.
So in general, I would say that Facial
paralysis associated with NF2 hits a bit
younger and that we have better results
with facial reanimation because of that.
But the other things specific to NF2 is
that both facial nerves are essentially
chronically at risk for facial paralysis.
So in unilateral facial paralysis, that
is based on an isolated brain tumor, an
isolated stroke a head and neck cancer,
or a benign parotid lesion, or something
that's only going to happen on one side
of the face and would be extraordinarily
unlikely to happen on the other side.
We depend on the
contralateral facial nerve.
For a lot of our facial reanimation
options in NF2 patients, we tend not
to do that as much because we don't
want to basically hang our hat on
normal contralateral facial function
for the rest of that patient's life.
So we tend to use more alternative
neural sources for facial
reanimation, if that makes sense.
Shane: Yeah.
So let's talk about that then.
There's essentially four options for
facial reanimation surgery, right?
If I'm understanding correctly,
could we step through each of
the modalities of treatment.
And then we can dive into each one in a
little bit more specifics, but let's just
do an overview of what are the options if
somebody is having facial paralysis for
treatment.
Dr Tessa Hadlock: Perfect.
This is my favorite subject.
So there are really two flavors
of facial paralysis that
NF2 patients can experience.
There is flaccid facial paralysis in
which there's been a sacrifice of the
facial nerve or very significant damage
in the skull base region where they
are not likely to experience recovery.
In the flaccid face, the
options are Threefold.
There's Static facial reanimation in
which we take fascia or tendon material
from other parts of the body and we
basically just provide some ribbons
underneath the skin that secure the
corner of the mouth and the appropriate
spot, the crease between the nose
and mouth and the appropriate spot.
We stabilize the central face so that
when people smile, things don't shoot over
to the healthy side and the that static.
Those, that static intervention
improves speech, articulation,
oral competence, keeping liquids
and solids inside the mouth.
It opens the nasal airway.
It does a lot of good things, but it's
not the sexiest thing that we can do
because it doesn't offer movement.
If we want to really introduce movement,
there are two main surgical options.
The first, which occurs when we can get
to patients within 6, 12, 18 months of
their paralysis, is to provide alternative
axons to the distal facial musculature.
And usually we will steal one of our
eight huge chewing nerves, which are
innervated by the trigeminal nerve,
very unlikely to be involved with NF2.
And we basically Cut one of those
chewing nerves and we sew it into a
relevant distal facial nerve branch
so that it brings back, let's say,
smiling with, at first patients do a
little small bite and then after a
while patients can learn to use that
without even clenching their teeth closed
and they can get a beautiful smile.
So those are called re
innervation techniques.
Stealing a different nerve to
plug it into the distal facial.
Nerve branches and actually
wake up the facial muscles.
Shane: So real quick, before we
go on, I want to take a step back
there from a lay perspective and
step through those two options.
just to make sure I'm
understanding their implications.
So in the first option, what you're really
doing is you're just creating tension
under the skin with with a tendon or some
other kind of non, I guess you could say
inert tissue that essentially pulls on
the musculature of the face at a certain
way that allows for symmetry to occur.
Because those muscles that
would normally be creating that
tension are completely, inactive.
And then in the second option,
you're actually grafting a nerve
from a nerve that supplies a
different set of muscles in the face.
And so the implication in that case,
if I'm understanding correctly, is that
actually They would need to, like you
were saying, a small bite or something.
They would need to learn, their
brain needs to learn a different set
of actions to activate that muscle.
Is that right?
Dr Tessa Hadlock: That is a hundred
percent correct, and you can think
of it as robbing Peter to pay Paul.
So I have to denervate one of the chewing
muscles to then to provide juice, if
you will, to some of the smiling muscles
or some of the periocular muscles.
But we only Rob people of muscles
that we know can be easily made
up for by other healthy muscles.
So in the end, people do not
wind up with new deficits in
order to restore facial movement.
Shane: That is a question I have
because, if you're making a small
kind of, change to one set of muscles
for the purposes of, or I guess one,
the nerve supply of a particular
muscle to affect a different one.
What are the knock on effects of that?
Even if they're small, do patients have
differences in the way that they chew or
differences in their kind of, mandibular
power when they're eating something, like
what do they need to be conscientious
of after treatment like that?
Okay,
Dr Tessa Hadlock: So there are two things.
When we use the masseteric branch of
the trigeminal nerve, which is the
really one of the most common nerves
that we use, People can experience two
things they have to be aware of and that
they might need a little therapy for.
One is that because we're taking away part
of the innervation of the masseter muscle,
they can get a little Temporomandibular
Joint Syndrome, a little TMJ.
So when they bite, they can
have a little bit of discomfort.
But luckily there are a lot of therapies
for TMJ, just in terms of warm compresses
and sometimes over the counter analgesics
and things like that, and a little bit
of changing in the diet so that we're not
doing crusty hard breads and stuff like
that, that can manage the potential TMJ.
The second thing that can happen, and
I see it a little bit more in wider
lower faces or an Asian kind of a
face where there's a wider bulk in
the masseter regions is that when we
take the nerve, it can almost look a
little bit hollow where the masseter
muscle gets a little bit atrophied.
In those cases, we can camouflage
that atrophy pretty easily.
with a little bit of filler therapy
or even a little dermal graft, which
is where we take a little piece of
not skin, but what's right under
the skin from, let's say the lower
belly or some inconspicuous spot.
And we make a little nick under
the skin and we drape in a little
bit of extra tissue so that we can
camouflage that volume deficit.
Shane: That's super interesting.
Okay.
Sorry.
So I interrupted you.
You were stepping through
the, these first two options.
And you mentioned there
were some other therapies.
Now these two therapies are related
to if the muscle in the, so the two
we just talked about are if the muscle
in the face is completely flaccid.
So they've completely lost function
Dr Tessa Hadlock: And there's no
real expectation for recovery.
The third option in that clinical
scenario is to do free muscle transfer.
Free muscle transfer means that we take
a muscle from elsewhere in the body
and we transplant it into the face.
And there are a number of muscles
that replace the smile musculature or
the periocular musculature, but the
most common one that we use is the
gracilis muscle from the inner thigh.
The reason we love that muscle is because
the scar is relatively inconspicuous
in the meat in the inner thigh, way
up so that even like a pair of shorts
would normally cover that incision.
And we so that therapy is appropriate
for people who have flaccid facial
paralysis for a prolonged period,
let's say more than 18 months.
In that scenario, you can provide
axons all you want, but it would
be very unlikely that the native
facial muscles would wake up when you
provided additional neural inputs.
That's not necessarily true in very
young children and even in young teens.
But as we get older, by the age of 15
or 18, after 18 months of deprivation
of neural input, we need to use a fresh
piece of muscle from somewhere else in
the body and transplant it into the face.
That's called free gristless transfer,
and we usually do that to restore
the smile, though we occasionally
are using it to also help people pull
down their lower lip in a pleasing way
when they want to expose full teeth.
for a big open mouth smile.
And there are also some descriptions
of providing the gracilis muscle in the
smile region and a slip underneath the
eyelids so that when we smile, we get
a little bit of elevation of the lower
eyelid that helps us protect our eye.
Shane: And then outside of that there are
sometimes, temporary treatments like Botox
that are appropriate for NF2 patients.
Could you talk a little bit about
when that might be appropriate and
what the implications of that might be?
Dr Tessa Hadlock: absolutely.
So we talked, we just talked about
therapy in the flaccid face, which
is one unfortunate sequela of, NF2
related management of vestibular
schwannomas or facial schwannomas.
But more commonly, or at least as
commonly in NF2, when the surgeons remove
a skull based tumor, they transiently
stun or damage the facial nerve and
a lot of recovery does then occur.
Remember, those patients are not flaccid.
But rather, they are, they can
be hyperkinetic, almost where
they recover, but there's no good
off button for that recovery.
So sometimes they wind up a
little bit too tight in the face.
So their facial muscles are
innervated by facial nerve fibers.
But, they're a little disorganized, so
a fiber that used to go to the smile
might now go to the eye muscle, or a
fiber that used to go down into the
neck goes up into the forehead, and so
those patients need really an entirely
different set of interventions to help
them organize their facial function.
And among the tools that we have
to manage that are Botox, which
for those of you who don't know,
basically temporarily disconnects a
nerve from a muscle to calm it down.
It just does that pharmacologically,
it doesn't do it anatomically.
So it wears off and it goes right
back to what we used to have, but
it basically can help inappropriate
activities disappear temporarily.
To improve function.
Physical therapy is an extraordinary
tool for that kind of hypertonic or
synkinetic phase, where a highly trained,
specialized physical therapist can help a
person to reprogram with neuroplasticity.
They're their cortex to better control
movements in a voluntary sense when
they want to make certain expressions.
So physical therapy, botulinum toxin,
which is really a medical therapy.
And then there are also some minor
surgical maneuvers that sometimes,
let's say, snip away a revved up
facial muscle that you never really
want to activate in the first place.
Like a little, there's a little frowning
muscle at the corner of the mouth that
we almost invariably want to throw
in the trash can because it hinders
smiling a lot after transient insults
to the facial nerve with aberrant
recovery and nobody ever misses it when
they can't make a huge downturn frown.
Shane: Okay so if I'm understanding
correctly, so we're talking about
after surgery or after some kind of,
resection that affects a facial nerve,
that nerve will sometimes grow back.
And as it grows back, it might
branch out and connect to the wrong
muscle or a different, musculature
than it was previously connected
to or should be connected to.
And that can cause, an activation
of a muscle that's unexpected when
a certain facial movement is done.
And you said something interesting
that I didn't realize was possible.
So a, so PT can actually be useful in
this case to cause somebody to unlearn
a particular facial, muscle activation.
Could you talk a little bit
more about how that works?
If if you're like PTS is not
an area that I'm, that I know
a ton about, that's also fine.
But that's something that's really
interesting to me because I, I think of,
and I think probably most people think
of most of our movements as intentional,
but involuntary in a sense, right?
Like we don't necessarily we do a
lot of movements in our face, but
we don't really think about which
muscles we're specifically activating.
And I wonder how that process works.
Dr Tessa Hadlock: I'll preface this by
saying that There are just a handful
of physical therapists in the country,
or maybe the list is even shorter than
that, who really can talk about the
very specific, , things that physical
therapy does more at a physiologic level.
But I I want to not correct you,
but add to what you're saying.
Facial expressions happen in two ways.
There are voluntary
expressions, a social smile.
Hi, it's nice to meet you.
And you smile intentionally.
You want to close your eyes because
you want to think hard about
something or keep the sunlight out.
Those are voluntary movements that we do.
There are also Involuntary, emotive
expressions that when somebody
says something funny and we laugh
out loud, we can't control those.
So there's a set of expressions that
we do control and a set that we don't.
And the pathway is totally different
where the voluntary expressions
come from the motor cortex.
In the cerebrum, the involuntary comes
through the amygdala and all this
kind of central core emotion pathways.
When physical therapists work to
try and do neuromuscular retraining,
they are able to take advantage
of the cortical plasticity.
The, basically that's our
brain's ability to reprogram.
certain voluntary motor
areas in the brain.
And it turns out that facial muscles
all the zones that control facial
muscles are all in very close proximity
to one another in the motor cortex.
And so getting those to cross talk by
repeatedly trying to make an action
and understanding what the action
does, and then trying to reprogram the
brain that way is relatively effective.
I am not certain, and I think it would
be interesting to have a physical
therapist do a podcast I think that
it would be interesting to know
whether the involuntary pathways
could be affected in a similar way.
Shane: Yeah, I really would like to get
some PT representation on the podcast.
Not just for, I mean, the
facial stuff is, is wild.
I hadn't actually even considered
that was an area of study.
Kind of specialization, but
just in general related to NF.
There's a ton of PT stuff related to
NF1, NF2 That I just don't think I know
a lot about, and I don't think that
kind of the community at large, I think
PT gets short shift in general, in the
same way that, in the same way that
mental health has a tendency to take a
back seat in these types of pathologies.
And I really want to
spend some time with that.
So if you have any names that you want
to throw my way that might be open,
I would absolutely love to reach out
and see if we can schedule somebody.
Dr Tessa Hadlock: A
hundred percent.
I'd be happy to do that for you.
Shane: do that.
I have a couple questions about specifics
of some of these procedures that I
want to explore a little further.
With the free muscle transfer, when you're
moving muscle from the thigh into the face
how much muscle are we really talking
about moving You know how much of material
are we actually taking from the thigh?
Does it affect the thigh
muscle at all, really?
Or is it such a small amount
that, it doesn't affect function?
And also how do you know how much
to move to achieve the effect that
you want to achieve in the face?
Dr Tessa Hadlock: So some
of those questions are known
and some are not known.
We do know that from just thousands
and thousands of gracilis removals
for all kinds of other reconstructions
around the body, that there really
is no significant morbidity to taking
out that muscle in the medial thigh.
We have really large other muscles
that perform the same action.
So the only time that we might hesitate
and even then only a little bit would be
like in a professional athlete who uses
their muscles to an extraordinary degree.
But other morbidity of removing this
little slip of what we really call a
vestige muscle from the thigh is minimal.
The question as to how much
to put in is a great one.
When I was learning these techniques
about 30 years ago, that we
had to put in 25 to 40 grams of
muscle in order to get movement.
But ultimately what people discovered was
that was frequently resulting in bulk or
visibility of that muscle in the face.
And over time, We systematically tracked
how little muscle we could put in and
still get an appropriate excursion.
Now, there's an element of
unpredictability in all of these facial
reanimation procedures, and so sometimes
there is not a direct correlation
with how much you put in and what
kind of smile excursion you get out.
And we've published an awful lot about
which variables predict the outcome.
And unfortunately, after 30 years
of doing this, I'm really still
all I recognize is how much more
there is to really study about that.
But I will say that we have
an upper limit of around 40.
15 grams of muscle that
we put in the face now.
So that means that when we take the
segment out of the leg, we have a sterile
scale in the operating room and we
weigh it and we assure ourselves that
we don't provide more mass than that.
Having said that, I have patients
with only six grams of muscle in
their face and a beautiful smile and
patients with 12 grams of muscle with
less excursion and a little bulk.
So there are clearly some variables that
we haven't been able to put our finger on.
Where we have made progress is let's
say we do this operation and somebody
winds up with a smile they're pleased
with, but the face is a little bit bulky.
We've gotten very comfortable in
correcting that bulk abnormality after
the fact in these kind of minor touch ups.
So we no longer feel that we're going
to put their whole reconstruction at
risk if we want to fix that one thing.
So there are many fewer things to
fear about the surgery than there
were, let's say, even a decade ago.
Shane: And that segues right
into, a little bit about
outcomes and success rates.
So for a procedure like this, and
I know probably each procedure
is going to have a different set
of considerations and stuff.
So feel free to go down
all those roads really.
, I really intend for these to be
as comprehensive as possible.
So don't feel like you're inundating
with too much information, but
with each of these procedures,
what are the considerations and
risks that need to be weighed?
And then I want to talk outcomes as
far as , long term outcomes keeping
in mind that disorders like NF2 come
with their own variability, of course,
but just in general, like if nothing
changed, what are the long term outcomes
for these various procedures as well?
Dr Tessa Hadlock: Yeah.
Okay.
So the first question is about risk.
And, in the NF2 population in
particular, these patients are
all facing intracranial disease.
Spinal disease and soft tissue disease
and nerves throughout the body.
And they often face.
Riskier surgery with craniotomy and pain
syndromes and all the kinds of things that
podcast is probably intended to cover.
So when it comes to facial reanimation,
I like to think, and I like to say to
patients that anything that we do to a
patient is so much less risky than all
of the other things that these guys have
to handle in the course of their care.
And that is, I would say, that is brought
out as a very honest statement over time.
It's not, the things that we do
not tend to be dangerous or have
really significant morbidity.
Has there been an occasional, I think
I can think of one patient in my career
that needed a blood transfusion after
surgery and a couple of people in whom
there were some rocky postoperative
courses, of course, but generally
speaking, the risks are very low.
The problem, the biggest risk with
facial reanimation is that it can fail.
And there are some patients.
who cannot accept that risk of failure.
And that's okay.
What that means is that they
shouldn't have facial reanimation.
So patients who come in, who hear
the options and say, I'm willing to
to get on board with this project
and roll these dice and get involved
with Tessa to try and make this
happen, that's a great candidate.
But a person who's been through either
very negative medical experiences
or has a very significant aversion
to the possibility something might
not work is somebody that we have
to we have to really consider very
carefully whether surgery is an option.
And I have a lot of NF2 patients who
at the outset of my proposing these
different things, they were like,
need time to process, and then over
time they come to appreciate or they
just become more comfortable with
the idea of the risk of failure.
And ultimately we proceed so with
free muscle transfer, at least,
there's really no time frame.
So we can take all the time that we
need together as a to really get to
a point where we know what the best
decision for that individual patient is.
In terms of long term outcomes, I
have spent my entire career trying
to meticulously track every single
facial reanimation procedure and its
short, middle, and long term outcome.
It's a massive undertaking.
I am pretty good at it, and I
still basically stink at it.
It's very hard to keep
track of these outcomes.
And particularly in the NF2 population,
because often people with NF2 will
travel to centers for their care.
So they start off with a particular
neuro oncologist and they come
back and that person follows them.
on a year over year basis.
And so they might get facial reanimation
with me because they're being
treated, let's say in the Boston area.
And I don't have as good access to them
when they go back to their home state to
follow photographs and clinician graded
outcomes measures and all of those things.
But I will, emphasize for you and
for your listeners that keeping
meticulous track of outcomes is the
most important thing that we can do.
And we owe it to the NF2 population
and we owe it to the facial
nerve population in general.
And no matter how many times I say
that over the course of my, I'm in the
senior years of my career It's still
very hard to to try to get clinicians
to, to do that and patients, and it's
not because they don't want to, it's
because the climate in medicine makes
it very difficult for people to take
the time to track patient reported
outcomes, clinician graded outcomes.
Layperson impressions of
outcome and objective outcomes.
It's time consuming, it's expensive,
and we as it is now don't have enough
time to spend with our patients.
Shane: Yeah, that makes sense.
But I do wonder just, in terms of patients
that you've had over the years, would you
say that, with most of these procedures,
excluding, say, Botox injection or other
temporary interventions, that these are
permanent or is this a situation where,
for instance, you do a nerve graft or
you do a muscle transfer and then in a
few years they may lose some of that
function for one reason or another is it
generally a permanent set of procedures
or is there a kind of infrequent need
for other procedures down the road?
Yeah,
Dr Tessa Hadlock: I understand
exactly what you're asking.
I would say in the case of
static reconstruction it is
Almost always successful.
And what I mean by successful is
they look a lot better at rest, maybe
70 percent better from an aesthetic
and functional perspective, but, and
it never really changes over time.
If you use the right materials
to do that, there are.
Some surgeons around the country who
use artificial materials and Gore
Tex and things like that and those do
not tend to have the same longevity.
But autologous materials like fascia
latae from the thigh or a palmaris longus
tendon and those things, what you get
is what you're always going to have.
And the only way that really gets
undone is if we have to cut it away
to access the area for other surgery.
When we talk about re innervation
procedures, also, we're Once I would say
that if we do that procedure within the
appropriate time frame, it's successful
far over 90 percent of the time.
When I mean , when I say successful,
I mean that they get dynamic movement
when they bite and in the face.
The spectrum of results can can occur
from exactly where those axons sprouted.
So because when we're doing that, we
can't stimulate the distal facial nerve
branches because they're not awake.
Sometimes we sew it to, A branch that
doesn't actually go exactly to the
smile muscles, but maybe a little
bit more vertically into the snarl
area, or maybe a little bit too much
into the eye or something like that.
So it's very successful at innervating
muscle, but it's not always
successful at the right targets.
And sometimes we need to do secondary
surgery to take down, let's say
they get a nice smile, but they
close their eye too much as well.
We can take down the
branch that does that.
Free muscle transfer in the
NF2 patient, which is also
driven by that chewing nerve.
92 percent of the time when I say work,
when people bite, they get a smile.
So that's the definition of success.
There are things that can happen that
then need secondary surgery to modify.
For example, occasionally the
muscle tightens a little bit too
much and the corner of the mouth
is a little bit too pulled at rest.
That's something that can be.
a little bit and adjusted.
Same thing with bulk, same thing.
If we do it and the vector
isn't exactly the vector that we
want, we can alter those things.
But as far as whether the operation
works 11 out of 12 times in my
hands and in a lot of, in an
experienced hands, it's going to work.
The trick is finding a very
experienced surgeon in this
because it's an unusual condition.
A lot of people say they do facial
reanimation and might have been trained
in a center where that occurred,
but the real learning happens in
repeatedly doing the operations.
And so you need to take the
time to identify people whose
volume then supports the results.
Shane: It's funny that this comes up
over and over again in my conversations,
which is the need for, experience
in specialization, because almost
all NF1, NF care in general is
specialized in a lot of these areas.
And I wonder if you see this
in your field at all as well.
When I talk to a lot of doctors they say
the issue is that there are experienced
clinicians, experienced surgeons,
experienced practitioners in general
in their fields, and they're retiring
and people are not filling their place.
There isn't a supply of other
practitioners interested in those.
specialties and coming in , as a freshman
class to keep that tradition going.
I'm wondering, in your field, are
you having the same problem a bit
of a brain drain within this facial
reanimation surgery, or is it something
that people are really excited about?
And you find that there's a lot
of people coming into it or a
lot of interest in it in general.
Dr Tessa Hadlock: Yes, I have the opposite
problem to most NF clinicians, which is
that I have a ton of people who are very
interested and I have a fellowship that
people apply for and spend a year with me.
And I would say there is almost too
much interest in facial reanimation.
When I say that, what I mean is that if
there are too many facial reanimation
specialists in the country, then no
single individual is generating the volume
that's going to make them excellent.
But so far in the past eight or nine
years, I've trained about 22 fellows
over my 22 year attending career.
And of, I would say in the past 10
years every graduate has gone back to
a major academic center eight in the
United States and two internationally.
And I think that we are starting to
stud the country with people who come
out of training at a high volume center
like mine and are capable of doing that.
Really becoming the next
generation of experts.
The problem is that there are also a lot
of other people, even at those centers,
who would like to do it because it's
such a captivating and alluring problem.
And that can tend to dilute the volume.
I am not a believer in diluted volume
for highly specialized problems.
Shane: I guess the upshot is that,
unlike a lot of NF specialized care, a
lot more patients probably have access
to this than they think, or that they
might initially assume without having
to say travel to Boston or something like
that, but it's interesting that there is
a balance to be struck between how many
practitioners are in the field versus.
How many actual procedures that need
to be done so that those practitioners
can become skilled enough To have
that level of expertise and I imagine
that impacts outcomes as well.
How often a procedure has to be followed
up with a secondary procedure because
one thing I wanted to ask about that
has come up a few times There's a
modicum of trial and error involved
is it just, having done enough procedures
to know when you're connecting a muscle
in a particular way, as you're performing
a graft or whatever, that you're
going to achieve a certain outcome.
How much of that is, okay, we're going
to do this procedure and then we need
to let it heal and we need to see
what happens and how much of that is,
technique that you can do during the
procedure to understand what the impact
is going to be and how does that work?
Dr Tessa Hadlock: Yeah, that's
a really nuanced question.
The way that I train Other
surgeons is in a very codified way.
And I think that I have learned through
mistakes the rights and wrongs of a
lot of these techniques and I am able
to convey that information very easily
to trainees as they come through.
The problem is that there is also a next
level of wisdom that comes from following
outcomes and trying to connect what you
did to what happens in the long run.
And with facial reanimation, clinicians
themselves, surgeons themselves are often
very ignorant of their own outcomes.
because they take so long to evolve
and clinicians are moving themselves
or patients don't follow up and
they're never getting those data back.
One thing I've tried to be extraordinarily
meticulous about since I have never
moved in my career from Boston is to
never lose track of a patient even
to the point where I'm contacting
patients who haven't come back so that
I get the answer to my own question.
What I would say is that There are things
that I have, there are insights I have
generated that I am able to articulate
and teach to other people so they don't
have to do the same 20, 30 years to learn.
But there are also things I
think that simply come with age.
And there, there was an article
written about, I think it was a
rhinoplasty surgeon or some other
type of facial plastic surgeon.
And a trainee was asking like, how
do you know what to do with the nose?
And the guy said, the nose talks to me.
And when I first read that as a young
clinician, I didn't really get it.
But as I've gotten older I almost.
Feel that same way.
Like the face talks to me, and
there are these very subtle things
that I'm doing that I'm not able to
articulate maybe to the people who
are around me, but that I think make
the result better in the long run.
I don't know if that
answers your question, but
Shane: In any kind of skilled
practice, there is an element there
that I think I totally get what you're
saying, which is that there's an
element of instinct that is built over
time that is, subconscious, right?
The brain, is.
So incredible at that, as you learn a
skill, there are just, there are things
that become, it's almost like when you're
first learning to drive a car, you're
thinking about every component of driving
the car and nothing is automatic and it's
very difficult and too much information
and then as you learn and, learn so much
of that becomes motor memory and, that's
where the training becomes important
because you can either commit it.
Bad habits to motor memory or, bad
technique to, that motor memory, and you
can become a bad driver that way, but
you can also unlearn and relearn things.
And that's just the way I think that
learning any skill works and mastery
of skill over time, especially something
as complicated and involved as surgery.
I think most surgeons would probably
say there is like an ineffable
quality to what they do in the field.
in addition to all of the quantifiable
tools that they use to make things
replicable and all that kind of stuff,
that just comes from the repetition
of that, and seeing the outcome.
And to your point I think that can
be, that a lot of surgeons they
kind of cut and move, and so they're
just moving on to the next procedure.
And that's a really good
point that you make.
And I don't know how many practitioners we
have that actually listen to this really.
I think the audience is mostly lay,
but I would really like, more of
that audience because I think that
is something that's lost sometimes,
which is the importance of.
Understanding the long term outcomes, not
just, the successful procedure and then
the next successful procedure and then
the next procedure, but also understanding
what the impacts to that are.
Because sometimes it's not just a
matter of successfully executing a
surgical procedure and then seeing how
the patient heals and then moving on.
It's also the execution of that procedure
with the consideration of the fact that
patient lives with that for the rest of
their lives and what the impact might be.
And there may be, something you can
do a little differently as you learn,
as time goes on, that improves quality
of life outcomes rather than just
clinical outcomes, if that makes sense.
And I think that because in plastic
surgery, you have to consider
those quality of life outcomes
as well, because that's one of
your clinical outcomes, right?
Dr Tessa Hadlock: Yeah, and I would
argue it's the most important one.
I think that in plastic surgery, in facial
plastic surgery, and in, in all kinds of
other reconstructive arenas, we've come
to appreciate that the most important
thing is how the patient feels, and so
that's really come higher up on our list.
I will say that It is so difficult
to track facial nerve outcomes, and
it's one reason why our field has
not accelerated to the same degree
as, say, breast reconstruction, or
limb reconstruction, or transgenders.
There are so many other surgeries
where the results are much more
immediate and we suffer without
those data, and it holds us back.
And I also think that because we
don't have immediate access to
those data, we sometimes may develop
misconceptions that stick with us forever.
And I'm reminded of a book that I have
just read that I'm really enthralled
with, this book called "Think Again."
I can't remember the author's
name, but we could look it up.
And the whole idea is that you need to
approach everything so scientifically,
even if you're really well developed
in your idea, you've got to be
able to rethink and ask yourself,
what if I did it a different way?
And I would say that in my own career,
I'm having a renaissance of asking
some of the fundamental questions of
like, How can I move this lip that's
a little bit too low that gives
them drooling or oral incompetence?
How can I move it up in a better way?
I think our responsibility is always
to deliver the best result that we can
and also on top of that to continue to
innovate and accept the areas that aren't
good enough or where we could improve and
try to apply our wisdom to those areas.
Shane: Yeah, absolutely.
The book you're talking about
is by Adam Grant, I think.
And , I think it's a pendulum swing in
society at large, but also in medicine
where, there is this pendulum in medicine
for increasing specialization that
just drills down, and then that creates
silos and it creates kind of isolation
between these specialties a little bit.
And then it's Oh, okay, now
we need coordinated care to
coordinate all these specialties.
But sometimes what really just needs to
happen is that people need to talk a lot
more and they need to communicate and,
those data need to permeate those barriers
between silos so that connections can
be made between different specialists
and different practitioners as well.
People have a tendency to get into
our own little bubbles , just to just
culturally, but also in specialty
fields people get into their own
little professional bubbles as well.
And it's a good reminder that, that's
what Symposia and all these, mechanisms
that are built to spread information and
create those connections are all about.
And it just shows how
really important they are.
A lot of practitioners are so busy
and they see things like conferences
and symposia and stuff as a luxury
that they would love to have time for.
But a lot of times they just don't, or
even just reading all the journals that
they'd want to read or going through, and
I think that that we're coming to a point
where we're realizing collectively that
stuff is equally as important sometimes
as the other continuous training that
you might do, just exposing yourself
to other ideas, other practitioners,
other people in your field and outside
of your field even, making connections
between those types of things.
Dr Tessa Hadlock: I could
not agree with you more.
And I sometimes I'm filled with
sort of a sadness about the way that
clinical medicine has devolved into
this frenzy of hyper specialized care.
And even when I was a trainee, this
is 30 years ago, we spent so much
more time just sitting around a
desk really thinking it through in a
group setting, and the power of group
thinking was much easier to apply.
I think that academic centers are tasked
with providing innovative care, yet
with all of the other pressures and
responsibilities and kind of promotional
expectations and service expectations
and even paperwork and reimbursement I
think that the entire system is actually
causing us to move away from the systems
that would really allow the breakthroughs.
And it's one reason why I recently
stepped away from mainstream
academia into a solo practice.
So I could actually hit the brakes
on some of that and almost by
the luxury of more thinking time.
Shane: Yeah, that's a really
interesting perspective.
There's always a tension between
creating systems that improve efficiency,
things like the NF consortium, stuff
like that, where it consolidates
research so that we're not doing the
same research over and over again.
And, spreading that information,
cause there's a certain inefficiency
with everybody kind of doing
their own thing and whatnot.
And how people communicate
becomes very sporadic and random.
So consolidating that stuff has its
value, but that pendulum can definitely
swing in the wrong direction and
it can get too far down that road.
And we can lose some of the spontaneous,
value that comes from just thinking
about something for a while or having The
breathing room to, talk through something
with another colleague or whatever.
All those little things.
Sometimes that slack in the
system is also really important.
And I think we're missing that.
We kind of rubber band back and forth
between realizing how important it is.
And then thinking, Oh no, now we've
built too much slack into the system.
We need to organize better and we
need to like streamline everything.
And it's just like, we go
back and forth between that.
But I hope we could kind of strike a
better balance that allows to maximize
both the benefits of organizational
efficiency while also benefits of
leaving that room, leaving that, that
headroom, and hopefully taking some of
the administrative burden off, cause
you're right, that is the biggest thing.
You talk to researchers and 70
percent of their job is administrative
at a Harvard or whatever.
When they get granted , they spend
half of that grant money just in
paperwork and making sure that all the
right people are looped into things.
Dr Tessa Hadlock: Like I had an
experience where this happened frequently
in the senior years of my research
projects, I would get a new idea.
And I would say to myself, Tessa,
get that idea out of your head.
You don't have time for that idea.
And that's not what we want
creative people to be doing.
I was like, Tessa, how dare you
indulge yourself in a new idea?
You've got to get back into the grind.
And so that's a sad, I think when
that, when somebody is at that
point, you have to pump the brakes
and say something's got to change.
Shane: Yeah, absolutely.
You said creative, and I think that
is also just one, one last note,
and then we can start to wrap up
here because we're out of time.
And I don't want to take
up too much of your time.
I know you're super busy.
But Is you called yourself
a, you said creative people.
I don't know how many medical
practitioners and surgeons think
of themselves as creative, think of
it as a creative endeavor, but there
really is a massive component of
it that requires the same level of,
creative thinking process that, a
lot of other creative fields require.
And I think if we thought of.
surgeons and some other, medical
practitioners as being in a creative
field, that might actually change the way
that we approach some of those things.
And we might change the way
that we value some of those.
Not strictly analytical modes of
thinking in medicine, because I think
that is really important, a really
important component, especially when
you're dealing with evolving disorders
that are really complicated, that have
a lot of different effects that aren't
necessarily related to the core disease,
like an NF, you have to be able to think
creatively to be able to make those
types of connections between, And that's
really how I wanted to think about
Dr Tessa Hadlock: I hear that.
I think that in facial plastic surgery
and other plastic surgery fields, I
would say that it draws in the creative
people because they first think of a
lot of what we do as like artistry.
And so there are a number of people
who are sculptors and who are painters
and are come from the artistic.
So they're creative in that certain
sort of three dimensional way.
And I think that to your point, Many
doctors and certainly many surgeons
can be very good if they're not
creative, but I don't think they can
be extraordinary unless they allow
and develop that piece of their brain.
They might be great followers
of technique, but they are not
going to change the face of care.
And that's really how I've
wanted to think of my own career.
Shane: It's that extra 10 percent
that they just may never quite get
to without that extra dimension.
Great.
I really appreciate you taking the time.
I don't want to take up any more of
it, but just in case there's anything
we didn't mention here that you'd like
to cover or anything that you want to
point listeners to before we close out.
Dr Tessa Hadlock: I think I would just
end with the final comment that patients
really do need to be their own advocates.
And it's often hard to say to your
neuro oncologist or somebody that
you're reviewing scans with who's
so delighted with your status.
or your lack of the lack of change
in volume of your tumors or tumor
burden or your nice response to drug
X or drug Y, you need to still find
the voice to say I am not expressing
myself adequately on the face.
And I think that it's the onus is on the
patients to have the courage to try and
identify resources for facial paralysis.
They're there.
I'm here.
Even if people aren't traveling to
Boston, we can help them navigate
their own local systems a lot better.
I would like to see I would like to
see people get good facial nerve care
and however we in the facial nerve
community can play a better role in that.
We're here to do that.
Shane: Yeah, that's a
good point to end on.
And it's one that we often end on
these conversations, which is how
important it is for NF patients
to be advocates for themselves.
And you don't know what you don't know.
So hopefully this interview, clues
a couple of people that weren't
thinking about facial reanimation
surgery as an option before.
They learn that it's something
that's available to them and
they can start to advocate for it
because just like any a person,
doctors also can't know everything.
Sometimes you just expect them to be
the experts that know everything, but the
reality is sometimes bringing an option to
the table that they hadn't considered can
be really important as a patient as well.
So thank you so much for taking the time.
It's been a really great conversation
and if there's any outside of your
website, if there's any other links,
social links or anything like that,
that you'd like me to put in there shoot
them over and I'll be happy to do that.
Dr Tessa Hadlock: Sounds totally awesome.
Shane: Well, that's it for this episode.
Thank you to Dr.
Tessa Hadlock for lending her time
and expertise and special thanks to
her staff for helping to sort out
some technical issues while we were
getting set up for the interview.
You can find all the show
notes, links and whatnot for
this episode on DecodingNF.Com.
You can find and interact with
Decoding NF on most social media.
Maybe leave a review on Apple
Podcasts--I hear it helps somehow.
And if you want to talk
to me, I am easy to reach.
Just shoot an email over
to shane@decodingnf.com.
And don't forget Patreon.com/DecodingNF.
It's just four bucks a month and you
support the future of decoding NF.
Thanks for listening and goodbye for now.
Creators and Guests